The Epidural
This is THE standard method for managing pain during childbirth. In France, almost 80% of women opt for this solution.
The epidural is used for vaginal deliveries as well as caesarean sections. Whether or not you choose to have an epidural, a pre-anaesthetic consultation is held at the end of the pregnancy to check that there will be no contraindications in the event of an emergency anaesthetic.
The anaesthetic is injected between two lumbar vertebrae through a thin tube called the catheter. The catheter remains in place so that medicines, if necessary, can be injected more easily.
The epidural process
Having an epidural is not an obligation. The epidural is performed on your request during delivery. To have enough time to act and have an effect on your contractions, it must not be performed too late. This is why it is most often inserted when the cervix is dilated between 3 cm and 8 cm.
In practice, the anaesthetist begins by examining you and checking that you have no contraindications. Lying on one side, standing or sitting, you have to turn your back to the anaesthetist. He or she will disinfect and perform a local anaesthetic on your lower back. After introducing a needle between two lumbar vertebrae, the anaesthetist inserts the catheter into the needle. The needle does not remain in your vertebral column; it is used to insert the catheter.
In theory, the epidural is not painful as the area is previously numbed with a local anaesthetic. This does not mean that you will not feel anxious due to the needle (even though you may not see it as your back will be turned to the doctor). The fact that you have to remain still during the procedure can also be unpleasant if you are in a lot of pain. You may feel, very briefly, small electrical sensations or sensitivity disorders in your legs or back during the procedure.
The insertion of the epidural usually takes five to 10 minutes.
The effects of the epidural
The purpose of the epidural is to eliminate pain without affecting any sensations. Dosage is increasingly accurate and personalised to enable the future mother to feel the birth of her child. It usually takes effect within 10 to 15 minutes of the injection and lasts approximately one to three hours. Depending on the duration of the birth, further injections may have to be given through the catheter. Some maternity wards have set up a “pump” system. In this case, after an initial injection, you can self-administer the medicine by pressing a button.
Once the epidural is in place, you will have to lie down even if you can still feel your legs as they may no longer support you and therefore cause you to fall. However, you can always lie on one side of your body or the other.
Some facilities offer a mobile epidural. It enables you to maintain mobility in your legs as the dosage and medicines are different. You can therefore continue to move about and walk during labour. You are equipped with a portable monitoring system to check the baby’s heart rate and you can call the midwife at any time.
Epidural contraindications
A number of disorders or infections can be caused by an epidural: skin infection on the lower back, blood clotting disorders and certain neurological problems.
During labour, other contraindications may cause the anaesthetist to refuse to administer it, such as the onset of fever, bleeding or a change in blood pressure.
Benefits
- Pain is greatly reduced or even eliminated for most women.
- After an epidural, you do not fall asleep or feel sleepy, so you consciously experience the birth. If it is managed correctly, you experience all of the sensations associated with a vaginal delivery.
Disadvantage
- The epidural does not have the desired effect in approximately 5% of cases. It can also lead to partial anaesthesia: one part of the body is numbed but not the other part. This may be due to an incorrectly placed catheter or to an incorrect dosage. The anaesthetist will be able to correct this.
- Some women experience itching during the epidural due to the composition of the medicine; this primarily concerns mobile epidurals.
- You cannot stand up because of a lack of feeling in your legs. Feeling gradually returns when the administration of the medicine has been completed. Generally, it is necessary to wait at least two hours after the removal of the epidural to stand up.
- Some women suffer from a headache after an epidural.
- Childbirth usually takes place lying down as you cannot remain standing. This increases the risk of giving birth with the use of instruments (vacuum extractors, forceps, etc.).
- Contractions are often less strong and sometimes the medical team may - with your agreement - inject oxytocin to make them stronger.
- Because of the anaesthetic, you will not feel well if you have to urinate. A urinary catheter is often inserted. This is a small plastic tube that is placed in the urethra to empty the bladder.
- Sometimes, the future mother’s blood pressure decreases too much due to the epidural medicine and the baby’s heart rate becomes too slow. The doctor may then decide to carry out a caesarean section to avoid the risks faced by the mother and the baby.
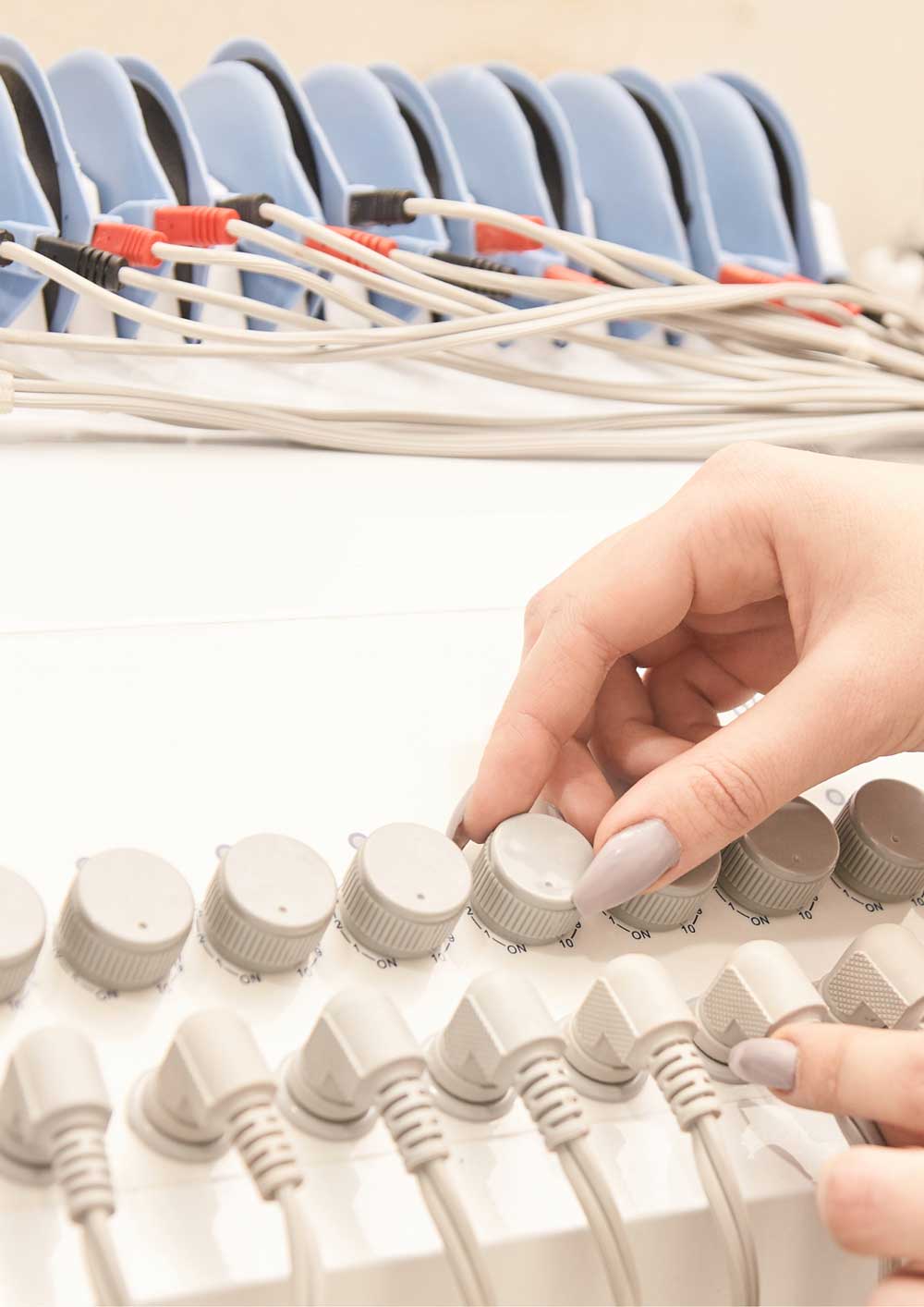
TENS or electrostimulation
This method, entirely under your control, consists of applying a low-intensity electric pulse to your back, causing a tingling sensation. This stimulation of nerves is intended to block painful impulses, encourage the release of pain-killing hormones (endorphins) and reduce anxiety. This method is considered to be particularly effective in relieving back pain.
TENS
Two electrodes are placed under the bra strap and two on the lower back. The electrodes are connected to the machine. You can choose the frequency and intensity of electrical stimulation using the control unit to get as much relief as possible.
Operation
At low stimulation intensity, the machine functions on the basis of “Gate Control Theory”. According to this theory, only a certain number of stimuli (or input) can be treated by the brain. There is therefore a “gate” through which only a certain amount of sensitive input can pass. Electrostimulation appears to create a “background noise” that occupies the input space available and thereby prevents the brain from noticing the pain caused by the contractions.
It appears that the mechanism is different when stimulation is higher. This is known as “diffuse noxious inhibitory control”. When the body is stimulated by a source of pain, it creates its own pain-killing hormones, called endorphins. The aim of electrostimulation is, therefore, to encourage the body to create its own analgesic. TENS appears to be more effective if you use it at the beginning of labour: endorphins are allowed to accumulate before the pain is too great.
The use of electrostimulation during childbirth also enables the future mother to feel more in control and reduce her level of anxiety.
Contraindications
There are no contraindications to electrostimulation.
Benefits
- You control the frequency and intensity of stimulation
- Electrostimulation has no impact on the baby or on the length of labour
Disadvantages
- The device cannot be used in the bath or shower
- Few facilities are equipped with these machines but you can rent or buy one
Analgesic gases
The inhalation of volatile gases as a form of pain relief during childbirth dates back to the middle of the 19th century, when ether and then chloroform were used. Nitrous oxide in combination with other gases was used for this purpose at the end of the 19th century. It is always mixed with oxygen so that the person can breathe. In countries such as Canada, the United Kingdom, Finland, Sweden or Australia, inhalation analgesia is used in 40% to 60% of births1 as an alternative to or prior to epidural anaesthesia.
It should be used during the active phase of labour if you do not want an epidural, if the epidural cannot be performed or while waiting for the epidural. Inhalation analgesia is also recommended during an episiotomy and its suture (with prior local anaesthesia).
How inhalation analgesia works: conscious sedation
You stay awake and inhale gas using a special valve called the “demand valve”. The gas is only dispensed when you inhale through the mask. This means that you have complete control over the administration process. If you remove the mask, you will not have any gas. Maximum effectiveness is achieved when you start to inhale around thirty seconds before the start of a contraction. It therefore requires some practice to identify the right time to breathe in the gas.
You should breathe normally through the mask until the contraction disappears. It takes about 50 seconds for the analgesic effect to be felt fully. You can remove the mask as soon as you no longer feel the contraction.
During conscious sedation, you are able to speak and react to your environment. The gas provides pain relief and also reduces anxiety.
Side effects
The most common side effects are dizziness, nausea, vomiting and dry mouth. You may also experience dreams, vague memories or ringing in the ears. These side effects disappear as soon as you stop inhaling the gas.
Contraindications
The use of analgesic gas is not advised when there is a history of epilepsy, cranial hypertension, obstructive pulmonary disease, bowel obstruction, otitis or sinusitis.
Benefits
- Inhalation analgesia is very easy to use.
- Inhalation analgesia significantly reduces pain when a contraction peaks.
- Contractions and labour are not affected.
- Inhalation analgesic is administered on request; you control inhalation and there is no risk of overdosing.
- The body eliminates the gas very quickly and it has no impact on the baby.
- Inhalation analgesia does not affect breastfeeding.
- Inhalation analgesia may be combined with other analgesics (opiates) under medical supervision.
Disadvantages
- Pain relief is lower than that provided by an epidural.
- It takes a little practice to know when to start inhaling the gas.
- The mask can make you feel claustrophobic.
- Not all maternity wards offer inhalation analgesia. Find out more during your prenatal visits.
So-called « natural » methods
Massage
Massage can help you relax your muscles and mind. It also distracts you from the pain. With some training, anyone can quickly learn how to massage. Some women appreciate it when someone constantly exerts pressure on their lower back. Others prefer to have their thighs massaged. Find out what you like. You may also not want anyone to touch you. In any case, share your wishes with your medical team and loved ones.
Relaxation, hypnosis
Hypnosis teaches you to relax your body completely, which can relieve pain. Despite this feeling of deep relaxation, you remain attentive and in control. If you would like to give birth under hypnosis, it is best to be accompanied by a hypnotherapist during your pregnancy.
To relax, some women enjoy using scented candles or scented oil. Others enjoy listening to music or other soothing sounds. The same principle applies here: do it if you find it comforting.
Acupuncture
Acupuncture is a traditional and gentle form of medicine that consists of placing thin needles into specific points of your body. These points are connected to places that are causing pain. Acupuncture can restore the body’s balance and reduce pain. Acupressure is similar to acupuncture but without any needles: only the hands or fingers are used. A third person (or you) exerts pressure on particular points that are connected to the place that is causing pain.
Benefits
- These methods are easy to use
- These methods have no negative effects on you or the baby
Inconvénients
- These methods may not be sufficient to relieve pain completely
- Not all facilities perform hypnosis or acupuncture. Find out in advance